Women with fibromyalgia (FM) have higher concentrations in the brain of a nerve cell receptor, called GABAA, that’s involved in the transmission of nerve impulses. These concentrations were associated with pain symptoms and impaired function, a study reveals.
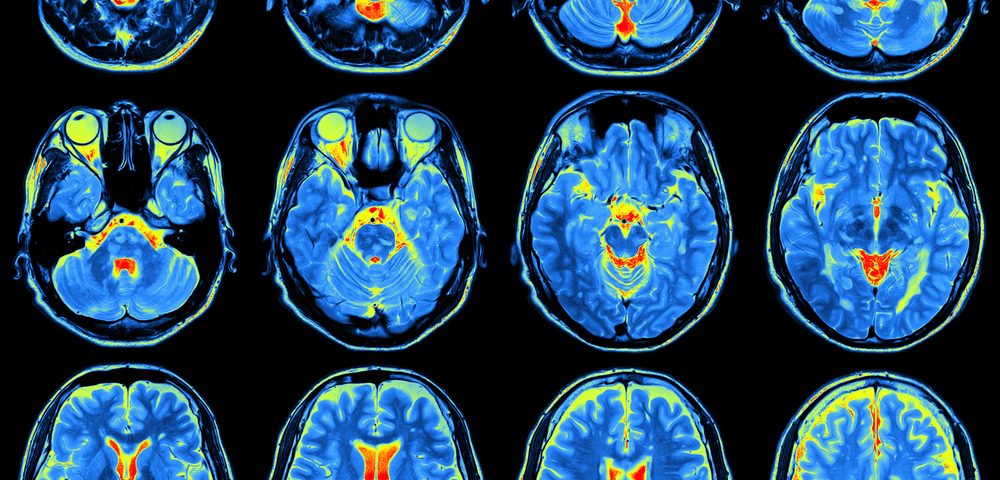
The findings, obtained through positron emission tomography or PET scans, suggest that GABA signaling — one of the most important transmission routes between nerve cells — is altered in the brain in people with FM. This alteration could possibly cause an imbalance between excitatory and inhibitory neuronal signals.
The study, “Up-regulation of cortical GABAA receptor concentration in fibromyalgia,” was published in the journal Pain.
Fibromyalgia (FM) is a chronic disease characterized by widespread pain, hypersensitivity, and cognitive and affective changes.
An increase in the excitatory versus inhibitory signals in the brain has been suggested to contribute to FM.
Brain analysis by magnetic resonance spectroscopy (MRS) revealed higher levels of glutamate, and reduced amounts of GABA, in certain regions of the brain cortex in people with FM. Both of these changes have been associated with increased sensitivity to pain.
Glutamate is the most abundant neurotransmitter — a molecule used by nerve cells to pass signals to other cells. It transmits excitatory signals, meaning it stimulates nerve cells to send nerve impulses.
In contrast, GABA is the main inhibitory neurotransmitter of the nervous system. Its principal role is to block the transmission of nerve impulses, to avoid too much activity of the system, which can be harmful.
Despite the available evidence, it remains unclear if the excitatory and inhibitory pathways of neurotransmission — the transmission of nerve impulses between nerve cells — are altered in people with FM.
To shed light on this, the researchers investigated whether women with FM have abnormalities in GABA signaling in the brain.
They quantified the concentration of the most important GABA receptor, GABAA, in the brain of 26 women with FM and 25 women without the disease, matched for age, physical activity, and body mass index. All women had already gone through menopause.
To measure GABAA receptors, the participants underwent brain scans by PET imaging, using a tracer for GABAA receptors, called [18F]flumazenil.
They also completed validated questionnaires, and underwent tests to assess pain sensitivity, attention, memory, and psychological status and function.
Compared with control participants, women with FM had increased sensitivity to pain and impairments in immediate memory. Specifically, they had a delay in recalling events.
Notably, these changes were accompanied by increased concentrations of GABAA receptors in specific brain structures of the FM patients, compared with controls. The affected brain structures included the right precuneus/cuneus, superior frontal gyrus, right angular gyrus, middle occipital cortex, inferior parietal/supramarginal gyrus, and lingual gyrus.
These are regions involved in self-awareness, consciousness, perception of emotions and sensory information, memory, attention, language, and visual processing.
No region showed significantly lower GABAA receptor levels in patients, compared with controls.
Across both groups, higher receptor concentration was associated with worse functional scores and greater pain intensity. But the pattern of these associations overlapped with regions with higher concentrations of GABAA receptors, providing a link between clinical outcomes and GABA signaling.
The findings show that people with FM have increased GABAA receptor concentrations, associated with pain symptoms and impaired function.
This increase most likely is driven by a higher number of GABAA receptors per nerve cell, and not by an overall rise in the number of nerve cells, the researchers said.
One important finding was that “the changes were widespread and not restricted to pain-processing regions,” the researchers said.
This finding adds evidence to the theory that FM patients have an imbalance between excitatory and inhibitory neurotransmission, which actually “seems to apply to different chronic pain conditions,” the researchers added.
“Since GABA is the most abundant neurotransmitter in the brain and is involved in a myriad of brain functions, an up-regulation of GABAA receptors across multiple brain regions could have important consequences,” they said.
According to the team, future research should focus on studying the change over time in glutamate and GABA, as well as their receptors, to disclose the root causes not only of FM, but also of other pain syndromes.