Scientists agree that central sensitization plays an important role in fibromyalgia (FM) pathology. A review study by Monash University researcher Geoffrey Littlejohn points out that peripheral neurogenic inflammation of the nerves also likely contributes to FM symptoms.
The review, titled “Neurogenic neuroinflammation in fibromyalgia and complex regional pain syndrome,“ appeared in the journal Nature Reviews Rheumatology.
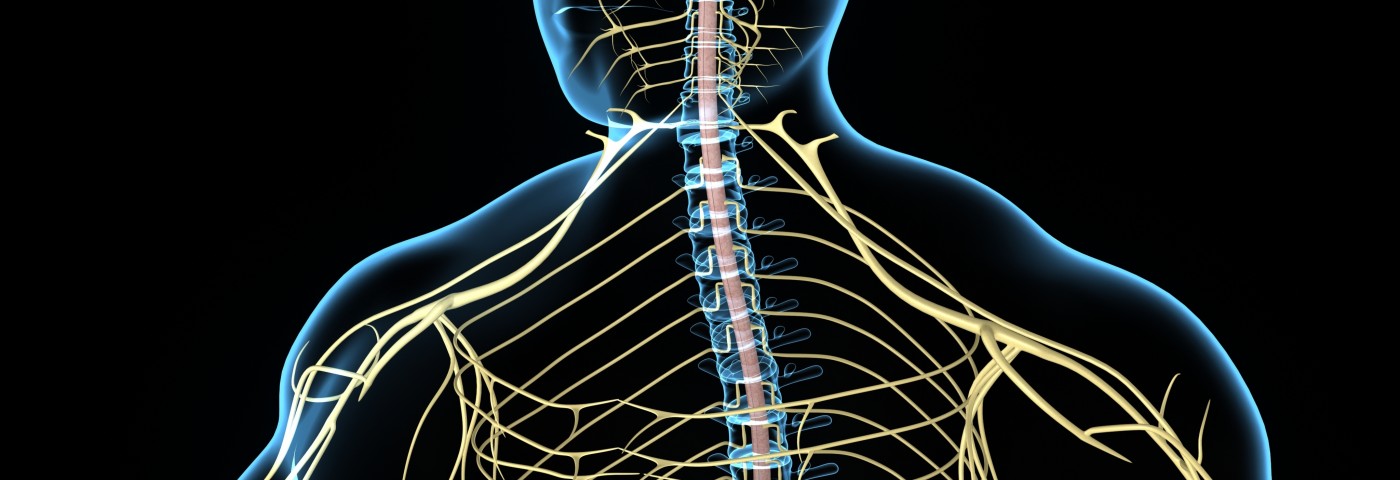
FM is considered to originate foremost from altered signaling in the brain and spinal cord. Central sensitization is a process by which nerve cells in the brain and spine become overly sensitive, responding with pain signals to normally non-painful stimuli.
In the peripheral nervous system, neurogenic inflammation is caused by the release of pro-inflammatory factors from the nerve endings of pain neurons. These factors, called neuropeptides, act on nearby blood vessels and attract immune cells that release pro-inflammatory cytokines. This sequence of events ultimately leads to the expression of more alpha-receptors, making the sympathetic nervous system overly sensitive — a well-known finding in FM patients.
The release of neuropeptides and subsequent cytokines likely contributes to neurogenic flares, or the abnormal skin responses in FM patients. Such inflammatory skin reactions have also been linked to dysfunctional blood vessel endothelial cells that allow blood plasma to leave the vessels after stimulation of the skin. This skin response is also influenced by the sympathetic nervous system. Moreover, mast cells that release histamine, a molecule normally released during allergic reactions, are increased in FM patients.
While much of the evidence of neurogenic inflammation in FM comes from small, selective, cross–sectional and comparative studies, the gathered evidence rather consistently supports the idea that neurogenic inflammation in the peripheral nervous system contributes to symptoms of FM.
There is, however, also evidence that altered activity in the central nervous system can, in itself, trigger peripheral neuroinflammation. This concept would explain the idea that neurogenic inflammation, and hence FM symptoms, can be brought about without any external pain triggers. Patients with FM also have lower numbers of myelinated peripheral neurons, likely contributing to altered pain perception.
The presence of cytokines has also been linked to an overactive stress response, and many specific cytokines are known to activate the body’s main stress response pathway — the hypothalamic-pituitary-adrenal axis. Patients with FM also have an increased sympathetic stress response, with high levels of emotional distress and reduced heart rate variability. Researchers are, however, in the dark about what exact influence the sympathetic nervous system has on neuroinflammation in FM.
Neurogenic inflammation involves a set of mechanisms interacting in complex ways. The integral components, nevertheless, constitute potential treatment targets. The stress response which is a likely contributor to the peripheral nerve inflammation can be targeted through education, exercise, and psychological interventions.
Some patients might benefit from drugs such as propranolol or phenoxybenzamine that decrease sympathetic nervous system activity. The interactions between stress and the central nervous system could be targeted by drugs such as gabapentinoids. It could also be possible to alter pathways from the brain to the periphery that control pain using drugs such as serotonin and noradrenaline reuptake inhibitors.
Neither glucocorticoids nor NSAIDs have shown any efficacy in FM, and there are no clinically available pharmaceutical options targeting neuropeptides found to be effective in FM treatment. Biologic drugs that target inflammatory cytokines, such as TNF, also have not proven to be beneficial.
Intravenous or subcutaneous polyvalent IgG therapy has been proposed for FM, but so far there is no convincing evidence of the treatment’s efficacy from randomized trials. Another approach yet to be confirmed in clinical studies is targeting the μ‑opioid receptor with naltrexone. The drug can reverse neural pain from chronic constrictive nerve injury.
Mitigating microglial responses by drugs such as ibudilast, and minocycline, might be another approach. Studies show promising effects of minocycline in animal models of FM. Using drugs, such as ketamine, that target NMDA receptors in microglia and the spinal cord is an interesting approach since the receptor is a known player in altered pain states. But again, there are no trials supporting such an approach. Targeting glutamate signaling in the brain and spinal cord using the drug memantine might also dampen neurogenic inflammation.
As already mentioned, much of the current knowledge of neurogenic inflammation in FM come from small or not well-designed studies. More research is needed to determine how much the peripheral inflammation of nerves contributes to FM. It is also important to establish whether neurogenic inflammation is a secondary effect of the disease or a stress-induced mechanism that drives the disease in its own right.
Targeting the above-mentioned points under clinical experimental conditions could lead to a better understanding of the mechanisms and aid in the development of FM treatments.