Increased levels of neuro-immune factors – implying activation of mast cells – in patients with fibromyalgia (FM) have been reported in a study published in the Journal of Pharmacology and Experimental Therapeutics.
The study, “Substance P, Hemokinin-1, CRH, TNF, and IL-6 are increased in serum of patients with Fibromyalgia Syndrome and may serve both as biomarkers and targets for treatment,“ offers new insight into FM pathology.
While the diagnostic criteria for FM has developed in the past 10 years, diagnostic or prognostic biomarkers would be of value in FM clinical management.
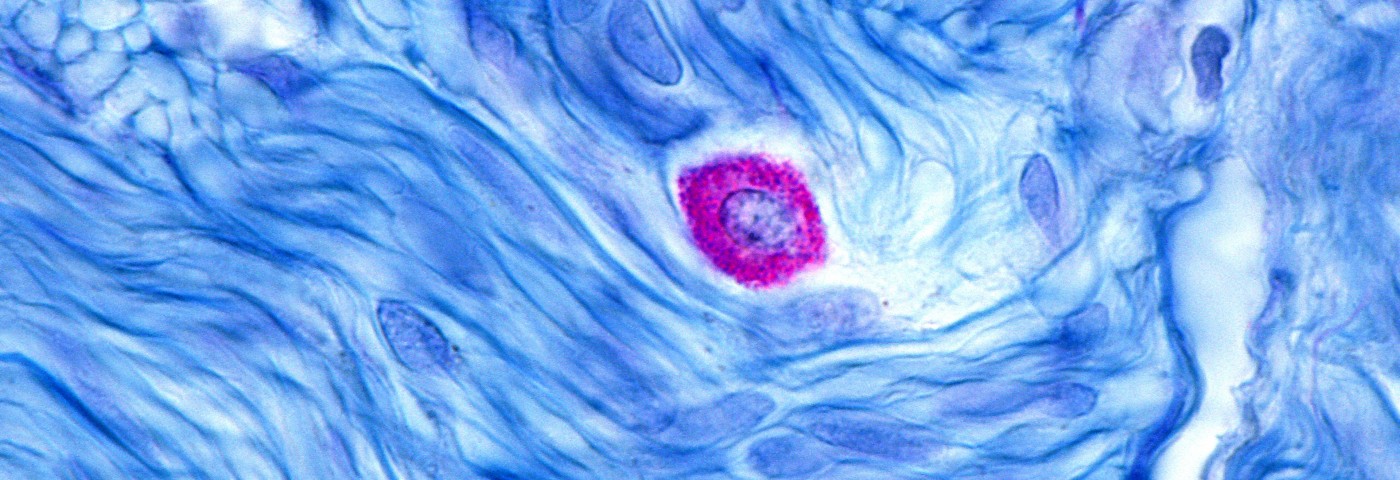
Scientists set out to identify factors that could act as biomarkers of the disease. Earlier research had shown that inflammatory mediators might be involved in FM pathology. Mast cells – immune cells guarding allergic reactions and possibly also systemic inflammation – have been proposed as central players in FM.
An earlier study reported increased numbers of mast cells in the skin of FM patients, but now, Irene Tsilioni and colleagues from Tufts University School of Medicine, Boston, believe that the level of mast cells’ activation might be more important than their actual numbers.
The team measured the levels of several factors known to be released by activated mast cells in the serum of 84 women diagnosed with FM. The levels of neuropeptides corticotropin-releasing hormone (CRH), substance P (SP) and Hemokinin-1 (HK-1), as well as the cytokines IL-6 and TNF, were elevated in the serum of patients compared to healthy controls. Levels of two other immune signaling factors – IL-31 and IL-33 – were lower in FM patients.
Previous research from the same group had shown that CRH and SP stimulate IL-6 and TNF release from mast cells, suggesting that neuropeptides could stimulate mast cells to secrete inflammatory cytokines that contribute to FM symptoms.
The authors argue that neuropeptides, likely released by the central nervous system, may cause the activation of mast cells throughout the body, leading to the inflammation and pain observed in FM. However, inflammatory factors may be released from mast cells in a circadian fashion, indicating that future studies should consider multiple sampling to achieve robust results.
The team argues that preventing the secretion of CRH, SP, and HK-1, and thereby stopping the release of IL-6 and TNF from mast cells, may constitute potential new treatment possibilities for FM.