High concentrations of two pro-inflammatory cytokines, interleukin 6 (IL-6) and IL-8, in fibromyalgia (FM) patients correlate with worsening clinical scores, suggesting that both cytokines may contribute to the severity of disease symptoms. These results, presented in a study titled “IL-8 and IL-6 primarily mediate the inflammatory response in fibromyalgia patients,” were published in the Journal of Neuroimmunology.
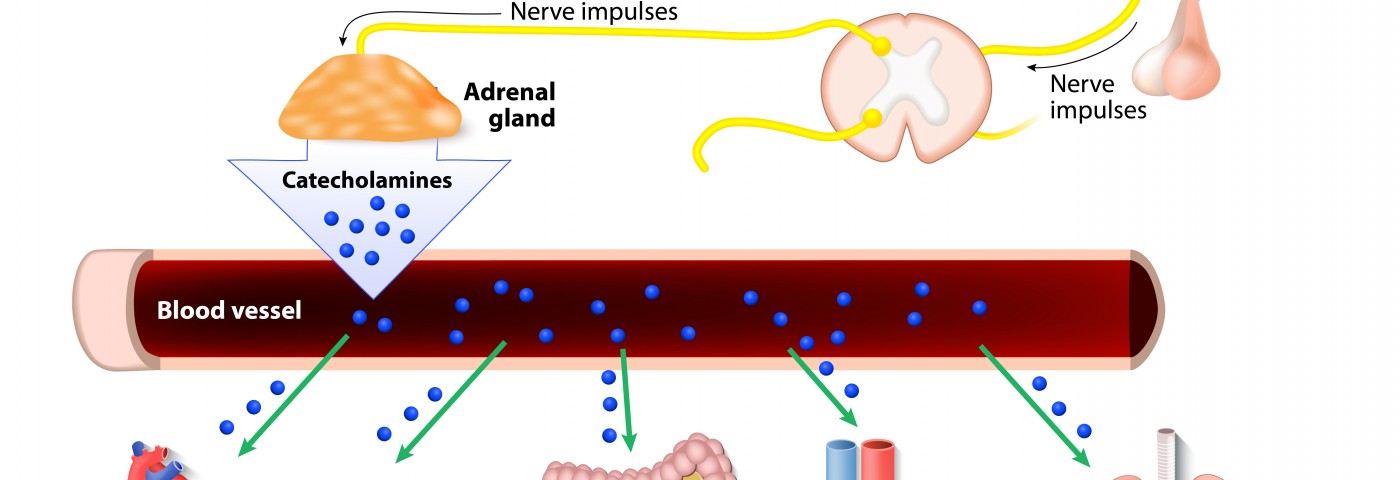
FM is a chronic disease characterized by widespread pain, tenderness, stiffness, fatigue, and sleep and mood disturbances. Affecting predominantly women (80% to 90% of FM patients), recent findings link FM to inflammatory reactions and alterations in body levels of pro-inflammatory cytokines, particularly at the hypothalamic-pituitary-adrenal (HPA) axis, a key network within the neuroendocrine system that regulates stress, digestion, immune responses, mood and emotions. In fact, it has been previously reported that cytokines influence several symptoms in FM patients, including fatigue, sleep, fever, and pain.
Researchers measured the levels of circulatory cytokines and how these correlated with FM patients’ psychiatric symptoms: serum concentrations of IL-2, IL-4, IL-6, IL-8, and IL-10; GM-CSF; IFN-γ; and TNF-α in both FM patients and healthy volunteers were recorded along with subjects’ psychiatric clinimetric scores.
A total of 15 patients at the outpatient clinic of the Instituto Nacional de Psiquiatría “Ramón de la Fuente Muñiz,” in Mexico City, were included in the study (out of 800 patients). FM diagnosis was confirmed by a rheumatologist, according to the 1990 American College of Rheumatology (ACR) criteria.
Researchers found that FM patients’ serum concentrations of IL-6 and IL-8 were increased when compared to healthy controls, and its levels correlated with psychiatric scales scores (the levels of other cytokines remained undetected in both FM patients and controls subjects). Although the study was performed with a low number of patients, these findings suggest that IL-6 and IL-8 cytokines may potentiate the pathogenesis of FM.
Additional studies with a larger cohort of patients and standardized conditions are required to confirm these preliminary results, and possibly translate them into clinical benefits for FM patients.