Fibrolmyalgia patients do not require periodical screens for celiac disease (CD), according to the results of a study titled “Celiac disease and fibromyalgia: Is there an association?” and published in The Spanish Journal of Gastroenterology.
Fibrolmyalgia (FM) patients are particularly burdened with CD and non-celiac gluten sensitivity (NCGS, a recent concept characterized by both gastrointestinal and extra-intestinal manifestations in the absence of CD or wheat allergy). Previous studies have suggested that FM patients with CD or NCGS given gluten-free diets exhibited fewer symptoms, including musculoskeletal pain and fatigue. However, it is important to determine which FM patients actually benefit from this potential therapeutic approach, a task that may prove difficult: not only can CD and NCGS be atypical and mild, but FM gastrointestinal symptoms are also commonly associated with irritable bowel syndrome. In fact, IBS patients show a significantly higher prevalence of CD compared to the general population.
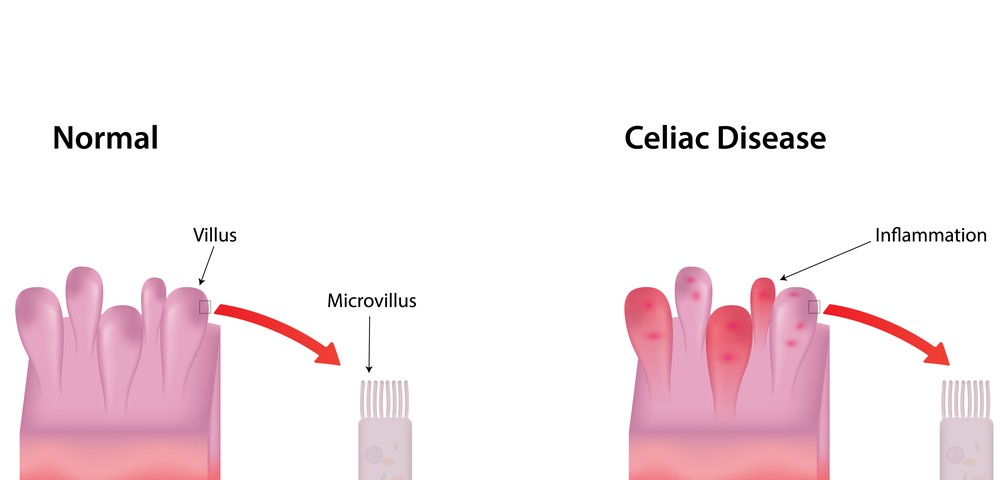
Researchers studied 188 women, 94 FM patients and 94 healthy controls, paired by age. They measured the levels of two diagnostic markers of CD, anti-transglutaminase and IgA endomysial antibodies. The results revealed only one FM patient (1.1%) tested positive for anti-transglutaminase, while all FM patients tested negative for IgA endomysial antibodies. As expected, all healthy controls were negative for both CD markers. The positive FM patient was subjected to a gastrointestinal endoscopy, and clinicians collected tissue from the patient’s bowel for a biopsy analysis. No histomorphological changes were found.
Given these results, authors discuss there is no need to screen every FM patient for CD. In a previous report, however, the same team found a 7% prevalence of CD and 56% prevalence of lymphocytic enteritis in duodenal biopsies of 104 FM patients with associated IBS. These discrepancies, they write, may be explained by differences in the prevalence of CD in the general population, known to vary according to geographical location.
The team concludes that searching for CD in FM patients should be restricted to patients exhibiting other signs of gastrointestinal diseases.