Combining two imaging techniques allowed researchers, for the first time, to visualize widespread inflammation, specifically mediated via glial cells, in the brains of fibromyalgia (FM) patients.
“Finding objective neurochemical changes in the brains of patients with fibromyalgia should help reduce the persistent stigma that many patients face, often being told their symptoms are imaginary and there’s nothing really wrong with them,” Marco Loggia, PhD, a researcher at the Massachusetts General Hospital-based Martinos Center for Biomedical Imaging and the study’s co-lead author, said in a press release.
“We don’t have good treatment options for fibromyalgia, so identifying a potential treatment target could lead to the development of innovative, more effective therapies,” he said.
Findings were published in the study, “Brain glial activation in fibromyalgia – A multi-site positron emission tomography investigation,” in the journal Brain, Behavior, and Immunity.
Despite increasing scientific evidence suggesting that inflammation in the brain — neuroinflammation — plays a role in fibromyalgia, no study until now had provided clear, visible proof of it in patients with the condition.
Earlier data from Eva Kosek, MD, PhD, co-senior author of the current study, at the Karolinska Institute in Sweden showed that fibromyalgia patients had increased levels of inflammatory proteins, namely fractalkine and interleukin-8, in their cerebrospinal fluid.
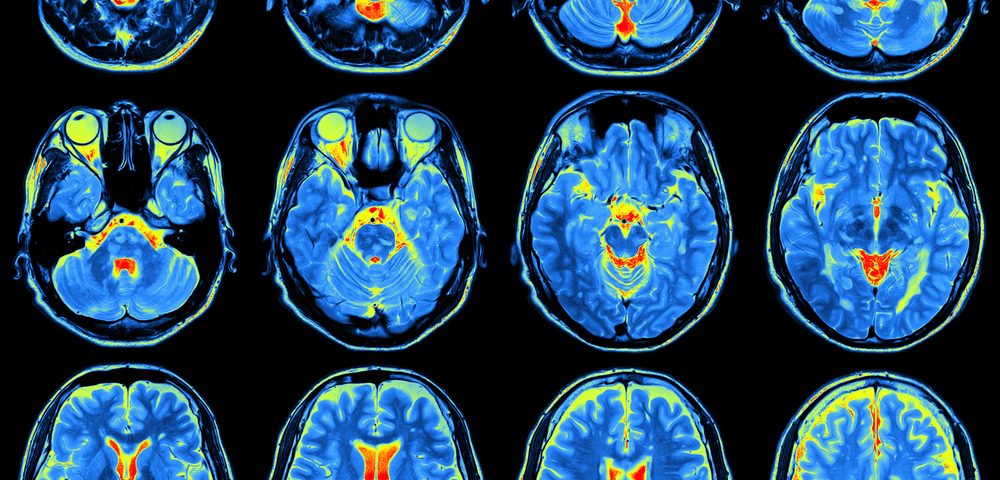
In 2015, Loggia’s team successfully imaged neuroinflammation — specifically the activation of glial cells — in the brains of patients with chronic pain using a new imaging approach — a combination of magnetic resonance imaging (MRI) and positron emission tomography (PET), or MR/PET scanning.
Glial cells surround the nerve cells in the central nervous system (the brain and spinal cord), and their main function is to support, protect, and nurture the neurons. The three types of glial cells found in the brain are microglia, astrocytes, and oligodendrocytes.
MR/PET blends the structural and functional detail of tissues that an MRI gives with the sensitivity and metabolic function that PET scans provide.
Specifically, PET scanning detects the radiation given off by a substance injected into a person, called a radiotracer, following its distribution throughout the body.
Loggia’s team hypothesized that fibromyalgia patients may also have activated glial cells, setting out to prove it using their PET strategy to image 20 fibromyalgia patients and 16 healthy volunteers. The radiotracer they used binds to the translocator protein (TSPO), a protein whose levels are increased in activated microglia and astrocytes.
Coincidentally, a similar approach was being designed by Kosek’s lab at the Karolinska Institute, where 11 fibromyalgia patients were enrolled for imaging, six of whom received the TSPO-binding PET tracer. Additionally, they had recruited 11 healthy individuals as controls who received a PET tracer that binds preferentially to astrocytes and not microglia.
Researchers at both institutes decided to combine their data sets — in total, they analyzed 31 fibromyalgia patients and 27 healthy controls.
The analyses revealed that the brains of fibromyalgia patients show significantly greater glial activation than healthy controls. Compared with the brains of patients with chronic pain, the increase of TSPO was more widespread in fibromyalgia patients. This may be an indicator of the more complex symptoms these patients have, according to Loggia.
Fibromyalgia patients who reported higher levels of fatigue showed higher TSPO levels in a structure called the cingulate gyrus, a region of the brain linked with emotional processing. These results suggest that “glial activation in this region as a potential mechanism underlying pathological fatigue,” the researchers wrote.
“The activation of glial cells we observed in our studies releases inflammatory mediators that are thought to sensitize pain pathways and contribute to symptoms such as fatigue,” said Loggia, who is also an assistant professor of radiology at Harvard Medical School. “The ability to join forces with our colleagues at Karolinska was fantastic, because combining our data and seeing similar results at both sites gives confidence to the reliability of our results.”
PET scanning using the astrocyte-binding tracer found little differences between fibromyalgia patients and healthy controls, supporting the idea that microglia are the key cells behind neuroinflammation in the patients.
“Our work provides the first in vivo evidence supporting a role for glial activation in FM pathophysiology,” the researchers said.
“Future studies will need to test whether glial modulation may be a viable therapeutic strategy for FM,” they concluded.