Fibromyalgia patients may have different cerebral blood flow parameters compared with the general population, according to a recent study. Researchers say these changes could be linked to clinical pain parameters and emotional factors.
The study titled, “Altered cerebral blood flow velocity features in fibromyalgia patients in resting-state conditions,” was published in the journal PLoS One.
Fibromyalgia is a chronic disease characterized by widespread musculoskeletal pain, an abnormal pain response from normally non-painful stimuli, and an excessive sensitivity to painful stimuli in many tender points. Several brain areas are activated in response to painful stimuli, and previous studies have shown that the brain networks during rest are altered in patients with chronic pain conditions compared with the general population.
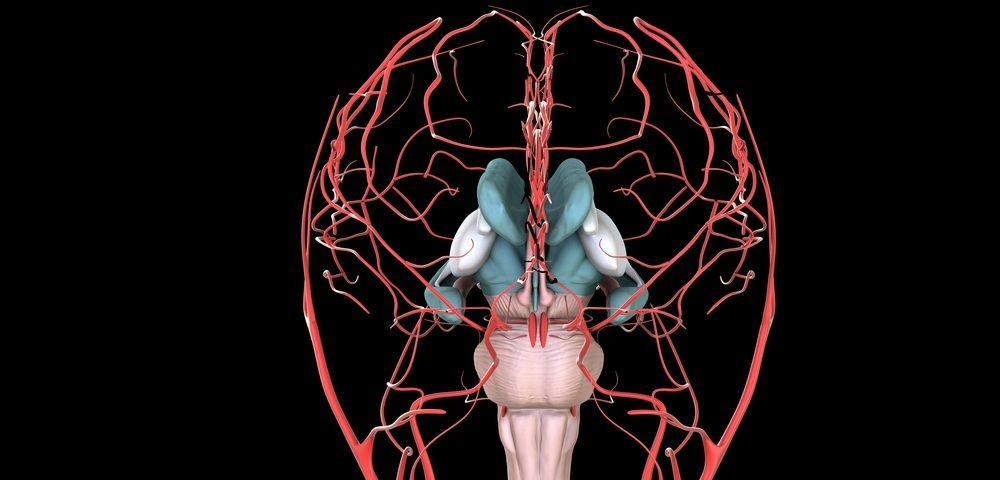
“One of the techniques that has been recently proposed to evaluate the dynamics of brain activation associated to painful stimuli is Transcranial Doppler (TCD) monitoring,” the researchers wrote. “It is a non-invasive ultrasound diagnosis technique that analyzes the [blood flow] variations in the brain by measuring cerebral blood flow velocities (CBFV) in main cerebral vessels.”
The study enrolled 15 women with fibromyalgia and 15 healthy women to investigate whether fibromyalgia is associated with changes in the brain, namely blood flow, during a five-minute, eyes-closed resting period. Researchers analyzed the anterior and middle cerebral arteries of both brain hemispheres in participants.
TCD monitoring showed that women with fibromyalgia presented a higher complexity of the CBFV signal.
Researchers also observed that women with fibromyalgia had significantly higher levels of depressiveness and anxiety than women without fibromyalgia, as well as significantly higher scores of pain intensity. CBFV changes were found to have a significant association with clinical pain parameters and emotional factors.
“All the obtained results are in accordance with previous studies that have demonstrated the relationship between negative emotional factors and activation of brain areas that are related to pain. Therefore, our results would confirm that the complexity and the frequency features of CBFV are linked with other factors such as the depression levels, the state and trait anxiety, and pain indicators of the participants,” researchers wrote.
Nonetheless, given the study’s limited number of participants and the fact that they were all women, the team emphasized that “the results should be confirmed with a large population of different age ranges and ethnicities, making possible to analyze the influence on the results of other related factors.”